Anatomy
The liver, the body’s largest organ, weighs about 1–1.5 kg and makes up 1.5–2.5% of lean body mass. Its size and shape typically reflect an individual’s overall body structure—long and lean or compact and square. It sits in the right upper abdomen beneath the lower rib cage, extending into the left upper abdomen, and is secured by ligaments connecting it to the diaphragm, peritoneum, major blood vessels, and digestive organs.
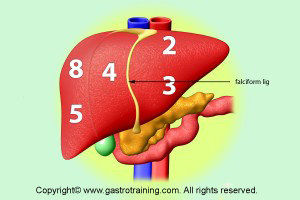
The falciform ligament on the diaphragmatic surface divides the liver into the larger right lobe and a smaller left lobe .
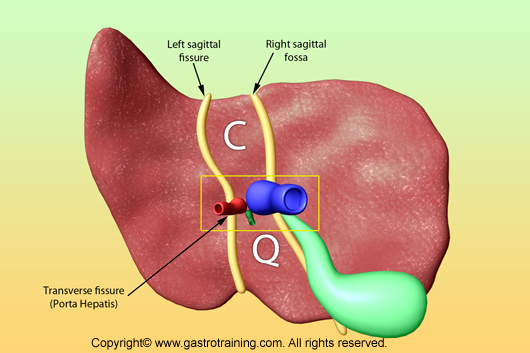
On the visceral surface of the liver, there is an H shaped group of fissures and fossa. The crossbar of the H is the porta hepatis (fissure for portal triad). It contains the portal vein, hepatic artery, hepatic ducts, nerves and lymphatics.
The left sagittal limb of the H is the fissures containing the ligamentum teres and the ligamentum venosum. The right sagittal limbs of the H are fossae for the gallbladder and IVC.
In this morphological description, the quadrate and caudate lobe belongs to the right lobe of the liv
Functional anatomy
Functionally the liver is divided into two lobes, right and left by a plane that passes through the gallbladder fossa and the fossa for IVC (i.e. left sagittal limb). Each lobe has its own arterial supply and venous and biliary drainage. Thus the caudate and most of quadrate lobe belong to the functional left lobe of liver.
Within each lobe the branches of portal vein and hepatic artery are consistent and divide each lobe into 4 vascular segments. So the liver is divided into eight functionally independent segments. Each segment has its own vascular inflow, outflow and biliary drainage. In the centre of each segment there is a branch of the portal vein, hepatic artery and bile duct. In the periphery of each segment there is vascular outflow through the hepatic veins.
Because of this division into self-contained units, each segment can be resected without damaging those remaining. For the liver to remain viable, resections must proceed along the vessels that define the peripheries of these segments.
Segment 1 (caudate lobe) is located posteriorly. It is not visible on a frontal view. On a normal frontal view the segments 6 and 7 are not visible because they are located more posteriorly. The right border of the liver is formed by segment 5 and 8. Although segment 4 is part of the left hemi liver, it is situated more to the right.
Right hepatic vein divides the right lobe into anterior and posterior segments
Middle hepatic vein divides the liver into right and left lobes. Left hepatic vein divides the left lobe into a medial (segment 4) and lateral part (segments 2 and 3). The right portal vein divides the right lobe of the liver into superior segments (7 and 8 ) and the inferior segments (5 and 6). During ultrasound it is easy to detect hepatic veins. Hepatic veins (RHV, MHV and LHV) divide longitudinally the planesand the portal vein (Righ and left) divide between cranial (7,8,4a and2) and caudal (6,5,4b and 3). This vascular structures helps identifying each segment.


Blood supply
The liver has a dual blood supply:
- 80% from nutrient-rich blood via the portal vein, which originates from the stomach, intestines, pancreas, and spleen.
- 20% comes from the oxygen-rich hepatic artery
Hepatocytes, the main liver cells, account for two-thirds of its mass. Other cells include Kupffer cells (from the immune system), stellate cells (fat-storing), and those of blood vessels and bile ducts.
Microscopically, the liver is divided into lobules, but functionally, it is structured into acini. Blood flows into the acinus from the portal areas (zone 1) and moves through sinusoids to the terminal hepatic veins (zone 3), while hepatocytes in zone 2 lie between these two. Viewing the liver this way explains many vascular and biliary disease patterns better than the lobular structure.

Portal areas contain veins, arteries, bile ducts, and lymphatics within a loose supportive matrix. Blood flows from zone 1 to zone 3 through sinusoids, draining into terminal veins, while bile flows in the opposite direction—from zone 3 to zone 1. Sinusoids are lined by endothelial cells with fenestrae that allow plasma, but not cells, to reach hepatocytes. Hepatocytes have distinct polarities: the basolateral side interfaces with the plasma in the space of Disse, while the apical side secretes bile into canaliculi that lead to bile ducts.
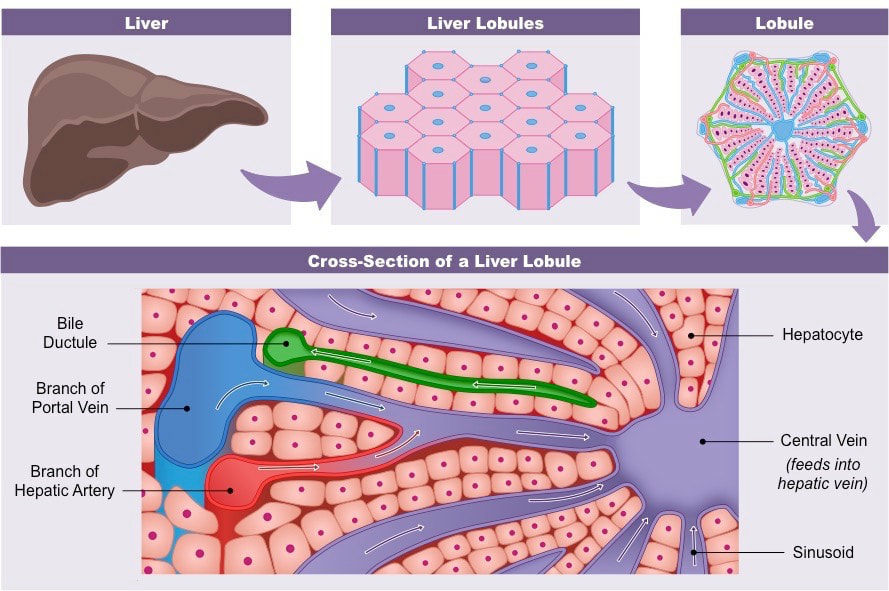
Kupffer cells, the body’s largest fixed macrophages, reside in the sinusoidal space, and stellate cells, which produce collagen and matrix when activated, lie in the space of Disse. Red blood cells remain in the sinusoidal space as blood flows through the liver while white blood cells can migrate through or around the endothelial cells into the space of Disse. From there, they may travel to portal areas and re-enter circulation via the lymphatic system.
Biliary drainage
-
Segments II, III, and IV–> Left hepatic duct
- Segments VI andVII (right right posterior sectoral duct : RPSD), coursing more horizontally–> Right hepatic duct
- Segments V and VIII: (right anterior sectoral duct RASD), coursing more vertically–>Right hepatic duct
- Segment I (Caudate lobe)–>drain into the angle of the left and right ducts. 15% drains into the left and <8% drains exclusively into the right

Liver function
Overview
Hepatocytes play a crucial role in maintaining the body’s balance and health. They synthesize essential serum proteins (like albumin, carrier proteins, and coagulation factors), produce bile and its components (bile acids, cholesterol, phospholipids), regulate nutrients (glucose, glycogen, lipids, cholesterol, amino acids), and metabolize lipophilic substances (such as bilirubin, drugs, and ions) for excretion through bile or urine.
Assessing liver function is challenging due to the wide range and variability of these processes. Common liver function tests include measuring serum bilirubin, serum albumin, and prothrombin time. Bilirubin levels reflect the liver’s ability to conjugate and excrete, while albumin levels and prothrombin time indicate protein synthesis. Abnormal results in these tests often signal liver dysfunction. Complete liver failure is fatal, as its complex functions cannot be replaced by medical devices or infused substances like hormones or proteins.
Protein synthesis
he liver’s most crucial protein is albumin, with 10–12g produced daily. Albumin plays a key role in transporting water-insoluble substances like bilirubin, hormones, and fatty acids. Low albumin levels (hypoalbuminaemia) are common in chronic liver disease and can also occur in severe illnesses, sepsis, or conditions where protein is lost through the bowel (protein-losing enteropathy) or kidneys (nephrotic syndrome).
Other important proteins synthesized there include transport proteins like transferrin and caeruloplasmin, α1-antitrypsin, alpha-fetoproteins, α2-macroglobulin, complement proteins, fibrinogen, and ferritin. The liver also produces acute-phase proteins, which are released in response to liver injury. These include C-reactive protein, ferritin, hepcidin, complement, caeruloplasmin, and fibrinogen.
Bile Production
Bile, produced by hepatocytes, is essential for excreting substances that the kidneys cannot and aids in lipid digestion and absorption through bile salts and acids. Liver produces and excretes about 600 ml per day. It is composed of water, electrolytes, bile salts, acids, cholesterol, bilirubin, and phospholipids. After being secreted into bile canaliculi, bile travels through ducts to the duodenum or is stored in the gallbladder. Once in the duodenum, bile participates in digestion by:
-
Emulsification of Fats: Bile contains bile salts and acids, which break large fat molecules into smaller droplets, increasing the surface area for digestive enzymes (like lipase from the pancreas) to act on. This process is called emulsification, and it helps make fats more accessible for digestion.
-
Aiding in Fat Absorption: Bile acids help form micelles, tiny structures that surround fat molecules. These micelles transport fats, cholesterol, and fat-soluble vitamins (A, D, E, and K) to the lining of the small intestine, where they are absorbed into the bloodstream.
After helping with the absortion of fats, some bile components are recycled through enterohepatic circulation( substances excreted in bile pass into the intestinal lumen, and then reabsorbed by the enterocytes and returned to the liver through the portal circulation.) Gut bacteria convert unused bile into bile acids, which are absorbed in the ileum and returned to the liver for reuse.
Bilirubin Metabolism
The liver is crucial in breaking down heme from hemolysis occurring throughout the body. Heme is converted to biliverdin, then to unconjugated bilirubin. The liver conjugates bilirubin through the UGT system, making it hydrophilic for excretion into bile or, in small amounts, blood, where it is filtered by the kidneys. Most conjugated bilirubin is excreted in feces, while some is converted by gut bacteria into urobilinogen for reabsorption and enterohepatic circulation.
Fat-Soluble Vitamin Storage and Metabolism
Fat-soluble vitamins reach the liver via intestinal absorption in chylomicrons or VLDL. The liver stores or metabolizes these vitamins, such as vitamin A, which is stored in Ito cells and oxidized into retinal or retinoic acid for secretion into bile. Vitamin D3 is hydroxylated by the liver’s CYP-450 system and further activated in the kidneys. Vitamin E is secreted back into circulation, while gamma-tocopherol is metabolized for excretion. Although vitamin K is not stored in the liver, it is crucial for liver enzyme gamma-glutamyl carboxylase, which aids in the coagulation of blood.
Amonnia
The livr is the main site of ammonia detoxification. Ammonia is created following the degradation of amino acids and is then converted to urea before excretion via the kidneys. Ammonia that is not broken down into urea is synthesised into glutamine.
Drug Metabolism
The liver metabolizes and detoxifies xenobiotics through lysosomes and biotransformation. This process mainly happens in hepatocyte smooth endoplasmic reticulum through two phases: Phase I involves oxidation, reduction, or hydrolysis by cytochrome P450 enzymes to make substances more hydrophilic. Phase II conjugates these metabolites with glucuronate, glutathione, or sulfate, further increasing their hydrophilicity for excretion via blood or bile. Glutathione conjugation is essential, and its depletion can lead to toxic build-up, such as in acetaminophen overdose. Drug metabolism is influenced by factors like age, gender, diseases, or genetics.
Coagulation
All of the coagulation factors involved in the generation of a fibrin clot are produced in the liver, except for FVIII, which is primarily synthesized by the hepatic endothelium and extrahepatic endothelial cells
All profibrinolytic and antifibrinolytic proteins are synthesized by the liver except tissue plasminogen activator (tPA) and PAI-1 which are synthesized by endothelial cells.
Protein C and S are primarily synthethised in liver and prevent excess coagulation and fibrin formation during secondary hemostasis. They are called ‘anticoagulants proteins’
Other Functions
The liver is involved in thyroid hormone function, converting T4 to T3. It also synthesizes nearly all plasma proteins, including albumin, binding globulins, and proteins related to blood clotting (except factor VIII).
Bibliography
Harrison’s Gastroenterology and Hepatology ; Authors, Dan L. Longo, Anthony S. Fauci ; Publisher, McGraw Hill Professional, 2010.
https://www.gastrotraining.com/
https://mysciencesquad.weebly.com/ib-hl-d3a2.html
https://radiologyassistant.nl/abdomen/liver/segmental-anatomy