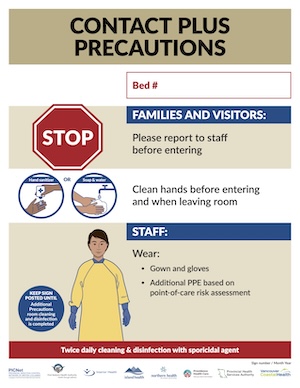
Epidemiologic precautions
The first part of the treatment is starting the necessary precautions to avoid further spread of the infections. This is isolating the patient, putting a sign on the door and maintain contact precautions (gloves and gown) for at least 48 hours after diarrhea has resolved
Medical treatment:
Initial Treatment for C. difficile Infections
- Preferred First-Line Treatment: If available, fidaxomicin should be administered at a dosage of 200 mg orally twice daily for 10 days, rather than vancomycin, for initial treatment.
- Alternative: If fidaxomicin is unavailable, oral vancomycin should be used at 125 mg every 6 hours for 10 days.
- Third-Line Option: If neither fidaxomicin nor vancomycin is available, oral metronidazole can be administered as an alternative.
- Subsequent Episodes: The European Society of Clinical Microbiology and Infectious Diseases (ESCMID) recommends fidaxomicin for subsequent episodes if it was not used initially. If fidaxomicin was previously administered, it can be repeated alongside bezlotoxumab ( human monoclonal antitoxin antibody; it binds to Clostridioides difficile toxin B and neutralises its activity) . For patients at high risk of recurrence where fidaxomicin is unavailable, bezlotoxumab should be added to the standard oral treatment for C. difficile infections.
Recommendations for Recurrent C. difficile Infections
- First Recurrence:
-
- Fidaxomicin: ESCMID recommends fidaxomicin as the preferred treatment in either a standard or extended-pulsed regimen, if available.
- Vancomycin Alternative: If fidaxomicin is unavailable, vancomycin is recommended. This can be given in a tapered and pulsed regimen or as a standard course:
-
-
- Initial 125 mg every 6 hours for 10–14 days,
- Followed by 125 mg every 12 hours for 7 days,
- Then once daily for 7 days,
- Finally, once every 2–3 days for 2 to 8 weeks.
-
- Additional Options:
-
- Fidaxomicin 200 mg every 12 hours for 10 days may be considered if vancomycin was used for the initial infection.
- Co-Intervention with Bezlotoxumab:
-
- According to the Infectious Diseases Society of America (IDSA), if recurrence happens within 6 months of the initial infection, bezlotoxumab should be administered along with standard-of-care (SoC) antibiotics, such as fidaxomicin or vancomycin.
- ESCMID also recommends bezlotoxumab as an adjunct to SoC for the initial recurrent episode.
Second or Subsequent Recurrence of C. difficile Infections
- Treatment Options:
-
- Tapered and pulsed vancomycin regimen: 125 mg every 6 hours for 10–14 days.
- Rifaximin: 400 mg orally three times daily for 20 days.
- Fidaxomicin: 200 mg twice daily for 10 days.
- Fecal microbiota transplantation (FMT) may be considered, especially for multiple recurrences unresponsive to antibiotic therapy.
Treatment for Initial Severe Infections
For patients with severe or fulminant C. difficile infection characterized by hypotension, shock, ileus, or toxic megacolon, the following treatments are recommended:
- Oral Fidaxomicin: 200 mg twice daily or
- Oral Vancomycin: 500 mg every 6 hours, given orally or via nasogastric tube if the patient has ileus. If needed, a rectal vancomycin enema (500 mg in 100 ml normal saline every 6 hours) can also be used.
- Intravenous Metronidazole: 500 mg every 8 hours as adjunctive therapy.
- Surgical Intervention: For cases of fulminant colitis with high risk for complications, such as toxic megacolon, intestinal perforation, or necrotizing colitis, subtotal colectomy with rectal preservation may be necessary. The ACG Clinical Guidelines suggest t either a total colectomy with an end ileostomy and a stapled rectal stump or a diverting loop ileostomy with colonic lavage and intraluminal vancomycin be used depending on clinical circumstances, the patient’s estimated tolerance to surgery, and the surgeon’s best judgment.

https://www.clinicalmicrobiologyandinfection.com/article/S1198-743X(21)00568-1/fulltext