The diagnosis is based on a series of clinical features that can be suggestive. The cardinal symptom is pyrosis (heartburn) that refers to a burning sensation usually ascending and behind the sternum. Chest pain and regurgitation are considered classic symptoms too. Normally, clinical response to PPI (proton pump inhibitors) is in itself a diagnostic feature and usually do not require additional test as long as there are no red flags (weight loss, dysphagia, palpable masses) or atypical symptoms (coughing, laryngeal reflux, dyspepsia). If any atypical/worrisome symptoms are present, gastroscopy should be perform first in order to rule out malignancy and to assess potential complications of reflux, such as macroscopic oesophagitis (10-50% of cases depending on the series) or Barrett’s oesophagus ( 5%–15% of patients with chronic GERD). Both features are indirect features of gastro-esophageal reflux disease as they are surrogate of mucosal damage.
Upper endoscopy is highly specific (90–95%) for GERD but has limited sensitivity (~50%). The extent and severity of mucosal injury can be assessed endoscopically.
Gastroscopy also can help assessing the anatomical region of LES and cardia , hiatal hernia, abnormal oesophageal diameter, lax lower oesophageal sphincter or slow gastric emptying. Avoiding gastroscopy in typical symptoms that respond to PPI is a universal approach based on general consensus and reflected on most international guidelines and associations, and the reason has to do with the high prevalence and the unaffordable cost and risk that would involve performing invasive tests to every symptomatic patient. Having said this, clinician must consider specific factors such as age, previous episodes, previous response to treatment, body habitus, risk factor such smoking, or family history . Additional test must be tailored to the patient clinical picture and needs. The guidelines of Lyon (2023) are the most specific for GERD. The modern definition of actionable GERD requires evidence of conclusive reflux-related pathology on endoscopy, and/or abnormalreflux monitoring in the presence of compatible troublesome symptoms.
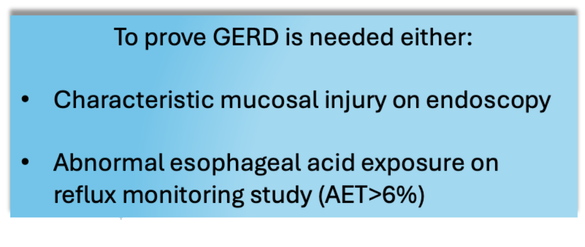
The gold standard diagnosis to confirm acid reflux is the Ph and Ph/impedance monitoring of the oesophagus. The demonstration of gastric content (usually acidic unless biliary content is abundant) into the oesophagus is based on 24 h nasal catheter that the patient carries home, or >48-96h in case of wireless Phmetry (Bravo capsule) for those patients who cannot tolerate the nasal catheter of the phmetry, in which case the Bravo capsule is introduced and fixed to the oesophageal wall via endoscope that self-detaches in a few days. In any case, distal electrode or the bravo capsule must be placed 5cm proximal (above) the LES. To know where the LES is, a manometry must be done usually on the same day. All these systems come with a recording device, usually in the shape of a small box which stores, views, and analyses oesophageal pH changes. PhMetry alone can only detect acid but not alkali reflux and cannot describe the direction or flow of the current change. However in the last decades it has become more popular the use of Impedance catheters with electrodes placed at 1-cm intervals which can detect changes in the resistance to flow of an electrical current ( impedance). Impedance increases in the presence of air and decreases in the presence of liquid bolus. This method can detect both gas and liquid movement in the oesophagus and used along pH electrode (all in the same probe) can detect the changes in Ph, differentiate alkali or acid reflux and discern between liquid or air content. In all cases the devices will be able to analyse the number or acid reflux episodes, the percentage over 24h, the association or not with patient’s symptoms, the predominant timing of episodes (daytime or nocturnal) and its relationship with food intake. This is very important because can differentiate between GERD ( Acid exposure time -AET- >6% or 80 episodes of reflux a day) reflux hypersensitivity (normal physiological AET <4% but associated with symptoms) or functional heartburn (normal AET and NO symptom association between the physiological acid episodes and when the patient logs the symptoms onto the machine). This is important because in functional heartburn there is no role for antisecretory medication. In general terms, patients who do not respond to antisecretory medication and lifestyle changes are the best candidates for a PhMetry study and manometry, as well as a gastroscopy if this has not been done. With all the information, the root cause can be better understood, and a range of treatment options may be offered.

These ambulatory monitoring tests are usually done off PPI and other antiacids (Unless wanted to monitor a well-known GERD patient with poor response to PPI in which cases it can be done whilst the person is actively on PPI). During this monitoring the patient must record the times of meals, sleep, and if any symptoms occur to them by logging this on the recorder (usually easily done by pressing a button).